Diagnosis
Many patients want to understand how doctors diagnose autoimmune hepatitis (AIH). We break down the complex process for diagnosing this rare disease.
Overview.
Diagnosing a patient with AIH can be difficult and in some cases take many months or even years. Since AIH is a rare disease, patients suspected of having liver disease will likely meet with a specialist called a gastroenterologist or a hepatologist.
Before a diagnosis of AIH is made, a hepatologist or gastroenterologist will rule out other causes of liver injury (for example, fatty liver disease) and may ask questions about alcohol and drug use including prescribed medications, vitamins, supplements, and recreational drugs to determine if these could have contributed to liver injury.
During your exam, your provider will likely ask about prior viral or bacterial infections, other autoimmune diseases you may have, and a medical history for first-degree relatives (parents, siblings, and children). The doctor will probably order blood tests to determine if you have ongoing liver inflammation (abnormal liver tests) or autoantibodies.

Abnormal liver tests.
The most important liver tests in AIH include alanine transaminase (ALT) and aspartate transaminase (AST), which are enzymes present in liver cells. Patients with AIH and active liver inflammation typically have liver cells that have been damaged by overactive immune cells. This causes ALT and AST to leak into the blood resulting in higher levels when blood work is performed. Patients without liver injury typically have low ALT and AST.
Autoantibodies.
Autoantibodies are proteins made by the immune system when it recognizes foreign material in the body. The presence of autoantibodies can help diagnose autoimmune disorders. In the case of AIH, antinuclear antibodies (ANA) and/or smooth muscle antibodies (SMA)/anti-actin antibodies are often, but not always, present.
Liver biopsy.
A liver biopsy is commonly ordered to help establish a diagnosis of AIH and to see if there is any scarring of the liver. It is typically performed by a radiologist.
Most biopsies are done by placing a needle into the liver through the abdomen (percutaneous biopsy); however, in certain cases a radiologist may take a biopsy from the liver by using a large vein in the patient’s neck (transjugular liver biopsy). In most hospitals, a radiologist will perform a liver biopsy by sampling tissue through the abdominal skin over the liver. This percutaneous approach is often completed with the use of numbing medication at the biopsy site. Intravenous medication may also be used to help patients relax. During the procedure, a small piece of liver tissue is removed, and a pathologist examines this tissue to determine if any scarring (fibrosis) is present and whether the patient has AIH.
FibroScan.
A FibroScan is a noninvasive test that doctors often use to track liver stiffness (fibrosis) in patients after diagnosis. It uses sound waves to measure liver stiffness painlessly. The test is not a replacement for a liver biopsy and has not been studied extensively in AIH patients. A FibroScan is not a reliable indication of fibrosis level when the liver has significant inflammation, which is why it’s not typically used when a patient is being diagnosed with AIH. Many doctors use FibroScans as a way to follow patients over time to ensure AIH treatment is optimal.
Types of AIH.
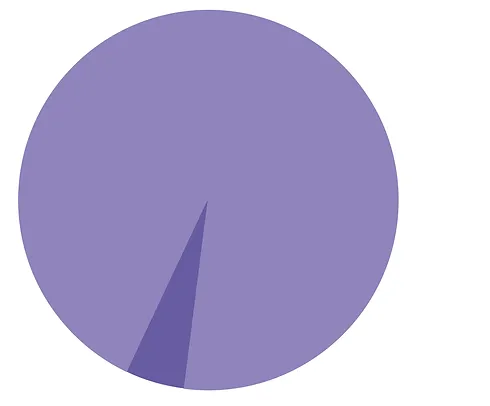
Type 1: 90%
Characterized by antinuclear antibodies (ANA) and/or smooth muscle antibodies (SMA)/anti-actin antibodies*. The onset can occur at any age, but it typically happens in adulthood.
Type 2: 10%
Characterized by antibodies to liver kidney microsome type 1 (anti-LKM1)*. The onset is more likely to occur at younger ages, and these patients usually require long-term immunosuppression.
*Up to 20 percent of patients may have seronegative AIH in which classic antibodies are absent.
